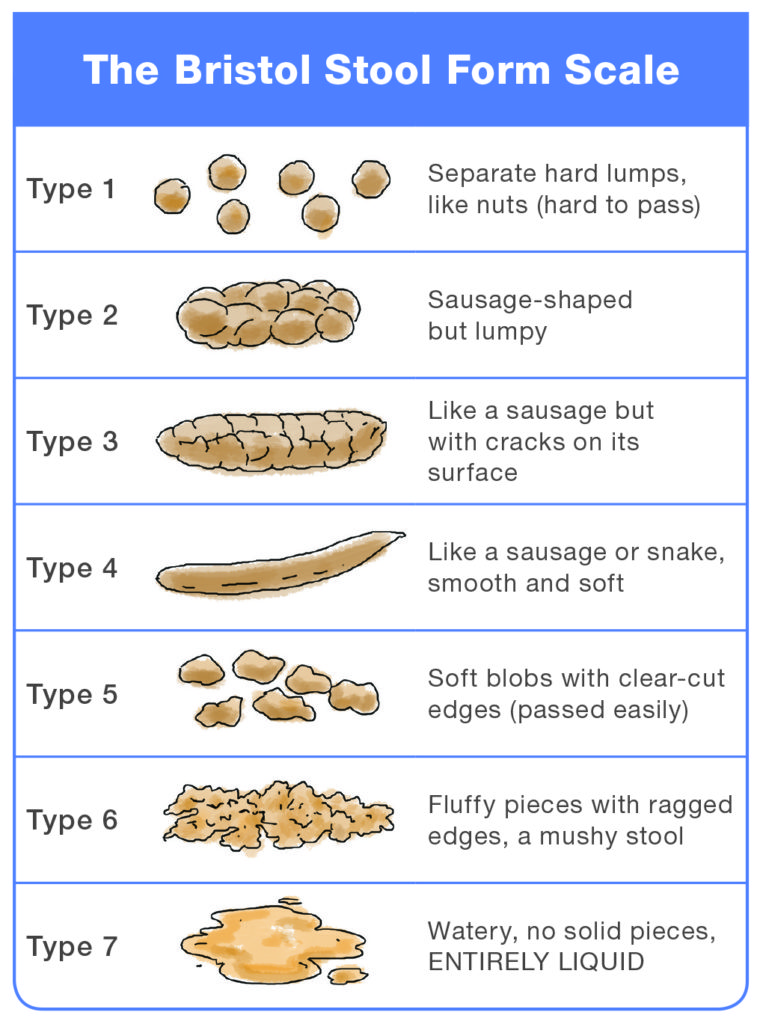
TYPE 1: Typical for acute dysbacteriosis. These stools lack a normal quality, because bacteria are missing and there is nothing to retain water. The lumps are hard and abrasive, the typical diameter ranges from 1 to 2 cm (0.4–0.8”), and they‘re painful to pass, because the lumps are hard and scratchy. Typical for post-antibiotic treatments and for people attempting fiber-free (low-carb) diets. Flatulence isn‘t likely, because fermentation of fiber isn‘t taking place.
TYPE 2: Represents a combination of Type 1 stools impacted into a single mass and lumped together by fiber components and some bacteria. Typical for organic constipation. The diameter is 3 to 4 cm (1.2–1.6”). This type is the most destructive by far because its size is near or exceeds the maximum opening of the anal canal‘s aperture (3.5 cm). It‘s bound to cause extreme straining during elimination, and most likely to cause anal canal laceration, hemorrhoidal prolapse, or diverticulosis. To attain this form, the stools must be in the colon for at least several weeks instead of the normal 72 hours. A person experiencing these stools is most likely to suffer from irritable bowel syndrome because of continuous pressure of large stools on the intestinal walls. The possibility of obstruction of the small intestine is high, because the large intestine is filled to capacity with stools.
TYPE 3: This form has all of the characteristics of Type 2 stools, but the transit time is faster, between one and two weeks. Typical for latent constipation. The diameter is 2 to 3.5 cm (0.8–1.4”). Irritable bowel syndrome is likely. Flatulence is minor, because of dysbacteriosis. The fact that it hasn‘t become as enlarged as Type 2 suggests that the defecations are regular. Straining is required. All of the adverse effects typical for Type 2 stools are likely for type 3, especially the rapid deterioration of haemorrhoidal disease.
TYPE 4: This form is normal for someone defecating once daily. The diameter is 1 to 2 cm (0.4–0.8”). The larger diameter suggests a longer transit time or a large amount of dietary fiber in the diet.
TYPE 5: This is an form ideal. It is typical for a person who has stools twice or three times daily, after major meals. The diameter is 1 to 1.5 cm (0.4–0.6”).
TYPE 6: This form is close to the margins of comfort in several respects. First, it may be difficult to control the urge, especially when you don‘t have immediate access to a bathroom. These kind of stools may suggest a slightly hyperactive colon (fast motility), excess dietary potassium, or sudden dehydration or spike in blood pressure related to stress (both cause the rapid release of water and potassium from blood plasma into the intestinal cavity). It can also indicate a hypersensitive personality prone to stress, too many spices, drinking water with a high mineral content, or the use of osmotic (mineral salts) laxatives.
TYPE 7: This is diarrhea, a subject outside the scope of this blog post with just one important and notable exception called paradoxical diarrhea. It‘s typical for people (especially young children and infirm or convalescing adults) affected by fecal impaction—a condition that follows or accompanies type 1 stools. During paradoxical diarrhea the liquid contents of the small intestine (up to 1.5–2 liters/quarts daily) have no place to go but down, because the large intestine is stuffed with impacted stools throughout its entire length. Some water gets absorbed, the rest accumulates in the rectum. The reason this type of diarrhea is called paradoxical is not because its nature isn‘t known or understood, but because being severely constipated and experiencing diarrhea all at once, is, indeed, a paradoxical situation. Unfortunately, it‘s all too common.
If you are looking to improve your stool quality our gutbiome test is a great place to start!